Mild Traumatic Brain Injury Can Cause Real and Long-Lasting Damage
Traumatic brain injury (TBI) is estimated to affect 1.6 million people in the United States each year [in 1991], and of these, 75% are classified as mild TBI (MTBI) [2003]. Many people with MTBI have difficulty returning to routine, daily activities and may be unable to return to work for many weeks or months. In addition to the human toll of these injuries, MTBI costs the nation nearly $17 billion each year.
There is no standard definition of MTBI even though injuries can be debilitating and long term.
“Mild” brain trauma is not necessarily insignificant – it’s merely at a smaller scale than hemorrhaging, contusions, edemas and the like. In situations where there is no external trauma to the head, such as whiplash in a car accident, the brain can collide with the interior of the skull, leaving little sign a trauma occurred.
When a client is seeking compensation and damages, there can be a bias that a person might exaggerate their symptoms when being examined by a neuropsychologist, so it’s important to be careful about who makes a diagnosis and that they consider multiple factors and interviews with associates. Receiving compensation and support for MTBI is an uphill battle when physical signs and non-exhaustive diagnosis reveal little to nothing, and you face insurance companies with deep pockets and lawyers on retainer who are determined to keep payouts low. More often than not, the deficits in affect and personality were much more detrimental to the patient than any cognitive deficits they experienced following the injury (Lezak, 1987; Lezak, & O’Brien, 1988). Without help, you may be struggling with work, mental performance, and treating your symptoms.
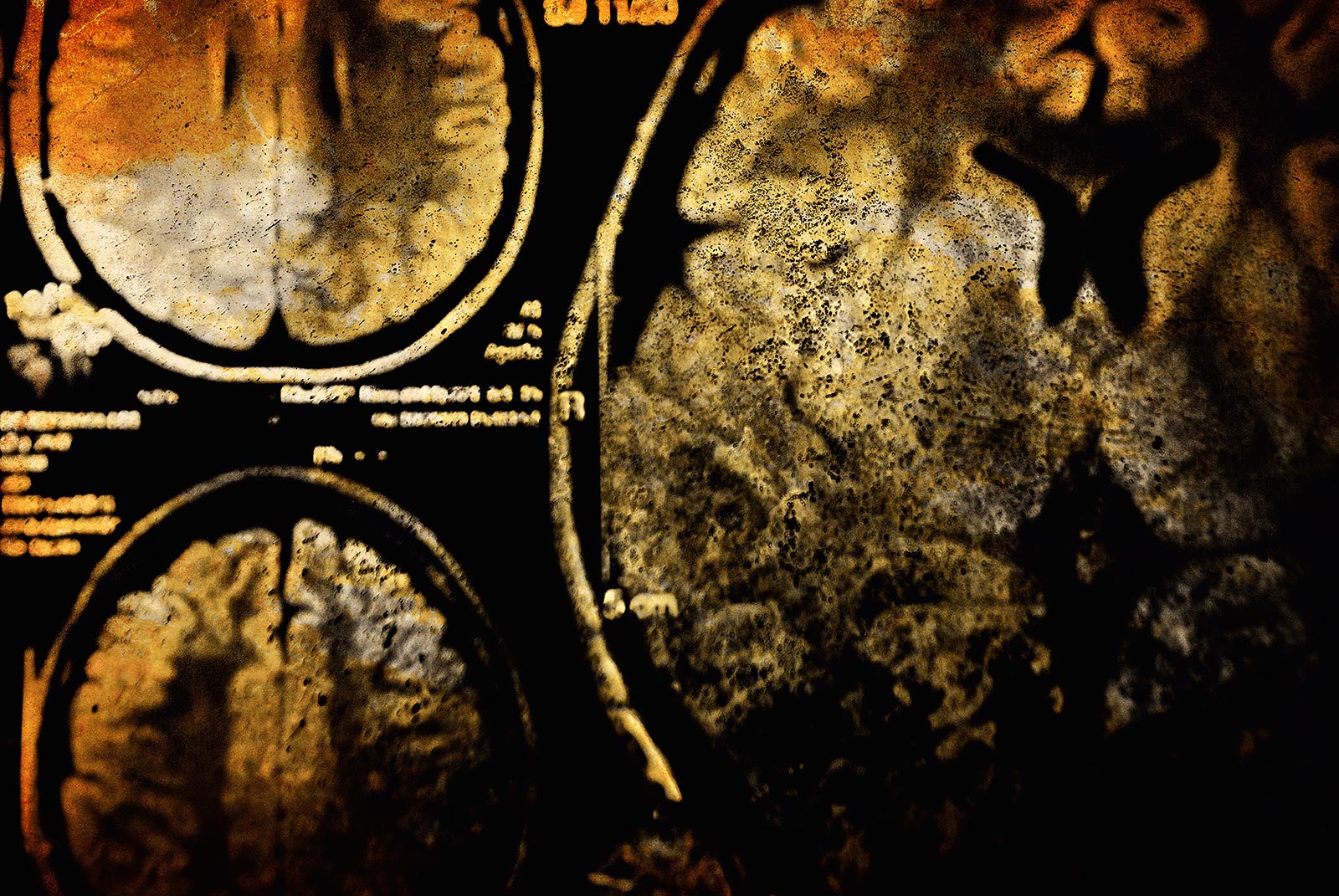
Litigating cases of Mild Traumatic Brain Injuries is complex. It is essential that patients document their treatment with appropriate neurologists and neuropsychologists as insurance companies will retain experts who may hold opinions that there will be no residual effects after 3 months of treatments. By definition, Mild Traumatic Brain Injuries do not typically show as physical abnormalities on CT and MRI scans. The MTBI sufferer can be accused of having all their pain and suffering “just in their head.”
As of 2017, nearly 5 million emergency department (ED) visits for head injury occur each year in the United States, of which <10% of patients show abnormal computed tomography (CT) findings. CT negative patients frequently suffer protracted somatic, behavioral, and neurocognitive dysfunction. Biomarkers can be used in addition to CT scans to detect potential non-visible trauma. Certain bio-markers like neuron-specific enolase (NSE) are elevated within 2-6 hours after an injury (with a half-life of 24 hours), meaning tests can be time sensitive [source , source]. CT scans performed within 3 hours of trauma may underestimate injury [source]. After 48-72 Hours, MRI is favored for use in trauma diagnosis. However, the overwhelming majority of patients with mild brain injury show no abnormality on MRI scans.
While many studies have shown that CT, MRI and other expensive scans are not necessary in all cases of head trauma, these regard reducing costs rather than eliminating the source of impairment and the costs in long-term disability, or that they are unnecessary because they do not show the fine structure damage.
